Today is the fifth anniversary of my brain surgery, I can’t quite believe that five years have passed. My hopes and expectations of returning to normal – going back to work, walking Dexter and generally living the same as I did before surgery – have long since dwindled away. Instead I’ve focused on creating a new life for the new Elaine.
People are sometimes confused by why I’ve not gone back to work or back to living my life the old way – going to the pub for example! Some often say “you’re looking well” or “you’re looking great”, I usually smile and say thank you because I know that they mean well. Damage to the brain is often invisible and, apart from my walking stick, I do look ‘normal’ and well! The reality is quite different, daily living holds many obstacles.
I wake up each day in pain, the location can vary, there never seems to be rhyme or reason to the pain. It’s neuropathic, caused by the damage to the nerves by the cyst. My arms, or legs, neck, back, shoulders, fingers, face, chest, collarbone can ache, burn, have shooting pains, to varying daily degrees. I also get abnormal sensations (dysesthesia) across my body. These range from burning sensations, itching, pins and needles, numbness, ice cold feeling under the skin, a wet sensation which I usually feel on my heels, as though I’ve stood in a puddle! I have a constant ringing, like a high pitched screech, in my right ear, it’s 24/7.
Mental and physical fatigue controls a large part of my life, limiting what I can do from day to day. Even though I pace myself to try and control it, because my brain and body compensate for my neurological deficits, I am constantly using more energy to complete simple tasks. Even standing uses more energy because my brain has to compensate for my posture and balance.
I sometimes get overwhelmed if two or more things need my attention, I struggle to structure my day and need to write down ‘to do’ steps to follow. I leave taps running, projects half finished because I’ve momentarily been distracted (usually Dexter barking at the postman or a stranger outside!) and I forget what I was doing.
Due to cerebellar ataxia I constantly feel off kilter, in a state of disequilibrium. Unsteady and imbalanced on my feet, with my spatial awareness feeling fuzzy, out of focus so that I can’t quite judge how close the wall is for example. I often put my arm out to steady myself or to gauge distance from objects. These feelings are magnified by distractions around me, this could be in the way of noise, crowds, busy roads or sometimes just someone walking towards me. Because of the nerve damage the brain can no longer receive messages from the receptors in my feet telling it what terrain or gradient I’m walking on, which allows the brain to send messages to adjust the posture and balance to stay upright on differing terrains and gradients. So I constantly need to watch where I’m walking because eyesight is the only way that the brain can know of any changes underfoot. This has its problems though, because filters in the brain that filter out noise and visual distractions no longer work, so if I hear or see something the brain stops focusing on walking and I, at best, stagger off course, or fall.
Despite all the daily challenges that I face, I get up and try to face each day positively and thankful that brain surgery was a success. I’m able to walk, talk, breathe and swallow, all the things that were at risk because of the cyst and all the things that I struggled and fought to regain after surgery. My breathing was laboured for several days after surgery, because the area of the brainstem that was affected, the medulla oblongata, controls our respiratory system amongst other life enabling functions. I remember reading an article about the medulla oblongata and surgery (thankfully I read it AFTER surgery!), it said that one wrong move near the medulla and the result is, at best a permanent vegetative state, at worse death. So I regard myself as very fortunate that I had an amazing, skilled surgeon who was willing to perform such a risk and to successfully remove the majority of the cyst wall from this fragile area. She has since retired and I wish her a happy and healthy retirement.
I had my yearly MRI scan in March and the results show no regrowth, the cleft that has been left in the brainstem looks stable and it was a thumbs up from the neurologist!
Life is harder but it is also simpler. I’m more appreciative of what and who I have in my life. During my recovery I have met some fantastic, supportive people and I’ve learned new skills which have helped towards building my new life.
I will be forever grateful for the care and support from the NHS, friends, colleagues, family, Lindsay’s family and, most importantly, from Lindsay who has been my rock, my cheerleader, my champion who believed in me and pushed me to achieve my goals and become the best Elaine that I could.
I know that I am unlikely to ever recover and be the Elaine that I use to be and I’m okay with that. These last five years I know that I have done everything that I could to become the best Elaine post surgery, so I can live with, and love, who I am today.
Category: Brain surgery
Regular Rehab Ends, A New Chapter in My Recovery Begins, A Sad Outcome (Part 12)
After seven months of regularly attending the rehabilitation unit, I had a review with the staff who were responsible for my rehab. They concluded that there was nothing else they could offer that I wasn’t already doing to improve my neurological deficits, I had reached the ceiling with regards to the therapy that they could provide. It was upsetting to think my time at rehab was ending, but I understood and accepted what they were saying. I had achieved so much and came so far in my recovery at rehab, but what I was doing there no longer challenged my brain or body.
They suggested that I explore courses that would target my neurological deficits. Christine, a support worker from rehab, took me to the North West Resource Centre which offered a variety of classes. We were introduced to a very helpful member of staff, Cathy Crompton, and once I explained to her why I was there and what my deficits were, she was able to suggest a selection of classes that would be ideal at focusing on, and hopefully improving those deficits. She suggested Tai Chi for my balance, coordination and mobility, I had been doing Tai Chi at rehab so I was delighted to be able to carry it on. She also thought that I should enrol in the quilting class as it could help with motor skills, dexterity and coordination. I told her I couldn’t sew at all, in fact if my work trousers lost their button I would go to the office and order a new pair instead of trying to mend them! However she talked me into enrolling in the next available class! Finally, she suggested a computer class as it might help with the neuro-fatigue and memory.
Once I knew I would have another avenue to go down to be able to continue working on my recovery, it helped ease the loss and sadness at leaving the rehab unit. The unit had played such a vital and major roll in my recovery journey, and I would always be grateful for the hard work and support that they had provided to get me to where I was in my recovery. On my last day they said that they would recall me in six weeks, so that they could monitor my progress and to see if I was adapting mentally and emotionally to this huge change. As sad as I was that this chapter of my journey had ended, I was also very happy because I saw it as a positive thing as it showed how far I had come, I was looking forward to the next chapter in my recovery!
I returned to rehab for my six week review and they were delighted with the progress I was making, and at the classes that I’d joined! They were happy to discharge me, but said they would like to recall me in six months, they don’t usually but they had grown fond of me and wanted to see my progress then! It was with a lump in my throat that I left rehab that day, but I was positive for the future.
I continued to go from strength to strength, the constant feeling in my head of imbalance and unsteadiness appeared to be lessening and there were times when I could walk without my stick! This was especially true at Tai Chi, I was managing to do most of the class without using my stick.
Sadly, when I returned to rehab six months later, they were alarmed and distraught at the deterioration that they saw in me. During those six months I had been put on Gabapentin for neuropathic pain, but within two weeks of being on the medication I had a sort of fit/funny turn when I was at the Resource Centre. I went into a daze and I lost control of my limbs, they were spasming and became extremely ataxic. I struggled to coordinate one foot in front of the other. It took three people to help me to someone’s car and get me back home. Thankfully Lindsay’s dad was there and he carried me into the house. He phoned his wife Lesley who came and phoned my doctor. He told me to stop taking the Gabapentin with immediate effect. He assured me that he didn’t think this fit was due to a reoccurence with the cyst, he explained that because the nerves in my brain stem are damaged, this would always cause malfunctions with the nerves causing them to misfire, which would cause miscommunication between brain, body, movement and normal functioning. And because Gabapentin targets the nerves to reduce the neurological pain, then this interference probably caused this funny turn, hence why he told me to stop taking it immediately. After this episode, my balance, coordination, motor skills, dexterity, speech, swallowing, cognitive awareness, fatigue amongst other aspects of my health, were significantly impacted and I experienced a huge deterioration in all areas. It was this deterioration that the rehab staff witnessed and were extremely concerned about. Even though I had been off the medication by this time for three weeks, there were no signs of me improving. The physiotherapist and nurse in charge were so concerned that they made an emergency appointment with the neurologist. He was concerned that there could be cysts along the spine so I was given an emergency full body MRI scan (until then I had only ever had a head MRI) which came back showing nothing. The neurologist suggested that I may of had an infection, he explained that any bug, infection or even tiredness would have a negative impact on my neurological deficits. He suggested that things would improve over time.
However, five months after stopping the Gabapentin, and two years since I’d had brain surgery, I had shown very little improvement when I went to see my neurosurgeon in Edinburgh. She concluded that the side effects from the gabapentin that I had suffered so severely from, were likely going to be permanent in my case. I was absolutely devastated. I had always said that, once I reached the two years (the figure they tell you that you will probably begin to plateau) if I still struggled with any neurological deficits and/or still needed to walk with a stick, then I would be okay with that because I would know that I had done everything I could, to become the best Elaine I could post surgery. But now that had all changed. I had reached the two year mark, and the deficits still impacted my day to day life, and I still needed to use a walking stick, but I had been on the verge of not needing it before I started on the medication, so I felt absolutely cheated. Sixteen months of gruelling therapy, hard work, determination and dedication had been wiped out within two weeks of being on Gabapentin. That appointment with the neurosurgeon was May 2017, and despite returning to rehab for further physiotherapy, to this day the level of recovery I had been at back in August 2016 before I started Gabapentin has never returned.
Goals, Proprioception and Neuroplasticity (Part 11)
After a couple of months of attending the rehabilitation unit I had a review, and during it I was encouraged to set goals. I told them I had two main goals that were important to me. The first was, I wanted to be able to attend my nieces’ wedding in August. The second was, I wanted to be able to walk my dog Dexter by myself, and I set a date that I wanted to be doing that by, which was 3/8/15.
To help me reach the goal of walking Dexter myself, an OT assistant visited to help me take him to the playing fields at the end of my street. I’ve mentioned in a previous blog that I had problems with bending forward, if I bent too far I would lose my balance and fall forward, and I could never judge when it would happen, one minute I’m okay and then the next minute this ‘klunk’ in my head would occur and I would fall forward! You are probably wondering why I’m making that random point in the middle of talking about walking my dog! It’s relevant because Dexter had a poo on this walk and the OT assistant was too squeamish to pick it up! So I said I would try but that I was worried I would bend too far and fall face first in dog muck! So she held on to the hood of my coat as I bent to pick it up!
My diary entry for that day (July 20th 2015) read: “I was so happy at managing the walk down to the playing field with only a few wobbles, it won’t be long before I’ll be walking Dexter on my own”. I then made a re-entry – under that original entry – on December 19th 2015, and this new entry said: “how wrong I was”. I had truly believed that I would be able to manage to go out on my own with Dexter within the next month or two, that the wobble that I spoke of would disappear once my balance had improved a bit more through the physiotherapy exercises I was doing. However, I go on to write in that second entry of December: “when I made the original comment I hadn’t been to visit Miss Myles (the neurosurgeon who operated on me). I had an appointment with her in the September and she explained the reason for the ‘wobble’”.
When I was at the appointment with Miss Myles I had told her that there had been several occasions when I would fall for no reason, it was as if my legs gave way. The worst time was when I was with Lesley (my partners mum) and I was trying to walk up an embankment to get a seat by the river. The moment I went to take a step up this slight embankment I crumbled to the floor. Lesley grabbed me and tried to help me back up but when I stood up the same thing happened. I bum shuffled back on to even ground, but I had no explanation for what had happened. Miss Myles explained it to me. As a result of the cyst stretching and damaging nerves in the brain stem and cerebellum, my proprioception had been impaired. I had never heard of proprioception before, but after learning what it meant it explained a lot of experiences I’d had before and after surgery. I will try my best to explain what proprioception means, although it took me a while to get my head around the meaning!
Proprioception is the sense of knowing where your body parts are in space. For example, if you were to close your eyes and wave your hand about, you will know where your hand is in space, even though it’s not being detected by any of the other senses. That made me remember the months before I knew about the cyst, I use to wake up and have the bizarre feeling of not knowing where my body was. I would lay in bed and look over my body and only then could I raise my arms or bring my legs out of the side of the bed. I use to think I’d drank too much the night before and my brain was still ‘alcohol foggy’!
Proprioceptors – sensory receptors located in muscles, tendons and joints – relay information about motion, tension and position to the brain and that’s what makes us aware of our body position and movement in space, these are unconscious processes. Without proprioception we would not be able to walk without watching where we put our feet. And that is why I kept falling or stumbling, and more so when I walked on uneven terrain or gradients, my brain wasn’t getting the information that there had been a change underfoot and so didn’t know to adjust my posture and balance to compensate for that. Miss Myles told me that my vision was the only thing that was giving my brain this information, so I needed to look at where I was walking at all times. Knowing this helped a bit with my mobility, but sadly, I also found that my brain didn’t just need to see, it also needs to concentrate on walking, so even if I’m looking at where I’m walking I still stumble, and this is because my brain can’t filter out sounds and sights. So, for example, if a car horn beeps, or a dog barks, my brain gets distracted by the sound and thus loses focus and attention on walking and that’s when I’ll stumble.
Miss Myles also warned me to be careful with the dark nights drawing in, as I would be more at risks of falls as the brain struggled to see where I was walking. This got me thinking, what would happen if I tried to walk with my eyes shut! Stupidly I tried it, if I stayed still with my eyes shut I was okay for a few seconds, but after that I started to sway. But if I tried to walk, it was the strangest thing, I couldn’t even lift my leg, when I tried it was as if there was a magnet attached keeping it locked to the floor. I told the physiotherapist what I had tried to do, she was horrified! She said I could have fallen and seriously hurt myself and not try do it again…I still try to do it to this day!
Miss Myles did offer hope with regard my neurological deficits, she said the brain was amazing in that it could rewire itself, this is known as neuroplasticity. So for the parts of the brain that were damaged, rewiring of the brain can make it possible for a function previously managed by that damaged area to be taken over by another undamaged area. It was likened to a diversion in a road. The quickest, smoothest route to get from A to B has a diversion in place. This diversion takes you a longer way round and along a bumpier, windier road, but it still gets you to your destination. So too, neurons in the brain create new pathways to compensate for the damaged pathways in order to carry out a task, it may take longer for that task to be done, and it may not be as efficient as before, but at least there is hope of completing it.
This appointment with Miss Myles helped me understand more about my neurological deficits, and offered me hope and made me more determined to do everything I could to become the best Elaine I could post-surgery.
The Rehabilitation Unit and Speech Therapy (Part 10)
In my previous blog, I touched upon going to rehab and speech therapy appointments, and I want to expand on these and explain how they helped me during my recovery.
On my first day at rehab I remember having to set the alarm early – I use to think nothing of getting up at 6am for work but since surgery I was sleeping right through to 11am most days as my brain recovered! I was picked up by patient transport just after 9am, I thought it would be too awkward taking my walking aid (Mavis!) so I used my walking stick that I used in my dog walking days! But I wasn’t very steady with it so the patient transport staff helped walk me to the bus as Lindsay waved me off! I’m quite a shy person (until you get to know me!) so as we approached the rehab unit I started to get butterflies. I didn’t really know what to expect and I felt very vulnerable, but I was immediately put at ease by the staff with their warm welcome and attentiveness. They introduced me to the other patients and helped settle my nerves.
On that first day, I saw Fiona, the physiotherapist, who did what’s called the BERG balance test which is used to determine the functional mobility of an individual, I would repeat it several times during my time at rehab to measure any improvement during my recovery. I also saw Leigh, the occupational therapist, whose primary goal is to help enable people to be able to participate in activities of everyday life, and so we looked at what activities I use to enjoy and did regularly (for example, cooking and walking Dexter) and then we worked on different therapies so I could hopefully do those things again. I also met Gillian, the nurse in charge, who helped with my emotional and mental wellbeing. The rehabilitation unit certainly offered a holistic approach, they didn’t just look at the physical impact my brain injury was having on me, but they recognised the impact it had on all aspects of my life – mentally, emotionally and even financially and they offered guidance, support and treatment tailor-made to my needs.
After several weeks of attending rehab once a week, Gillian decided I should try attending twice a week. I was really excited by this as I saw it as a big step in my recovery. Sadly though, it became apparent that fatigue was impacting on my recovery, the more I strived to do, the worse the fatigue became. And so, the decision was made that I would return to once a week. When Gillian told me I burst into tears. I was disappointed that I couldn’t manage the two days but normally I would never have cried about it! But fatigue played havoc with my emotions and I would burst into tears from sheer exhaustion. Fatigue didn’t just affect my emotions, it also affected my speech, swallowing and balance. My speech became more slurred and I struggled to get my words out right, I choked more often and I wobbled/stumbled off balance more when I was tired. Gillian kept telling me to pace myself, but in the early days I struggled with that because I kept thinking, the more I try to do the quicker I will get better. It took a long time for me to relinquish that stubborn mindset!
I started noticing something that hadn’t been apparent in the first few weeks after surgery, I never felt hungry or thirsty. I think because I had the feeding tube for the first ten days, and then meals were provided at set times after that in the hospital, and then Lindsay had made my meals for me once I got home. So it wasn’t until Lindsay returned to work six weeks after my surgery that it came to light. She would get home and would ask me what I’d had for lunch, and I would realise I hadn’t had lunch, in fact I’d had nothing to eat all day. She asked if I’d not been hungry and that’s when I realised that I never felt hungry or thirsty.
I also kept forgetting if I’d done things, when Lindsay got home she would ask me what I’d done that day, and I wasn’t always sure. I would question myself as to whether I had done my daily speech and physio exercises. With my head full of worries about forgetting to eat and drink, and not sure if I was remembering to do all my exercises, I went to my speech therapy appointment. Linda, the speech therapist, picked up very quickly that something was bothering me that day. So instead of concentrating on swallowing and speaking exercises, Linda helped me by listening to my concerns and then offering advice on how to resolve them. She suggested I create a timetable that would prompt me during the day to eat, drink and do my speech and physio exercises. She also said by following the timetable it would help structure my day. She was full of encouragement about how much I had already achieved. It was a beautiful demonstration of person-centred care by Linda, she was interested in the well-being of her patient and recognised, at that time, that I needed a listening ear, guidance and encouragement much more than I needed an hour of speech therapy. It was exactly what I needed that day and I left that appointment with renewed determination and motivation for my recovery journey.
Once I got home from the appointment, I began to draw a timetable but then I was concerned I would forget to look at it! So instead, I downloaded an app that allowed me to set and name several alarms to go off throughout the day. Here’s a screenshot of some of the daily alarms!

I then drew up a checklist so I could record what I was eating, drinking and when I was doing my speech and physio exercises, and Linda was right, it did help to structure my day and it also helped me feel I was accomplishing something each day with regards my therapy exercises, and so acted as a motivator to keep going! Thank you Linda!
Rehabilitation, Relearning, New Glasses and Goodbye Hair…(part 9 of I’m a 40-year-old blogger virgin!)
Once home I was so grateful that Lindsay had been given a couple of weeks off work from the doctor to help take care of me, she was a godsend – and still is. At home I coped pretty well with Mavis (the name I had given my rollator, walking aid!). Lindsay had transformed our downstairs spare room/darts room into a bedroom as I wasn’t able to climb the stairs. Dexter, our dog, soon learned to shift when I was on the move, I think that was after I accidently ran over his tail…he’s a quick learner!
A couple of days after being home I had an appointment with an optometrist who provided me with glasses that had a prism in the lens to compensate my double vision (a result of too much pressure to my eyes from lying face down during surgery). Lindsay refused to be seen with me as the glasses were so hideous! So she frog-marched me to her work and got me a better pair! I was just grateful I no longer had to wear the black eye patch!
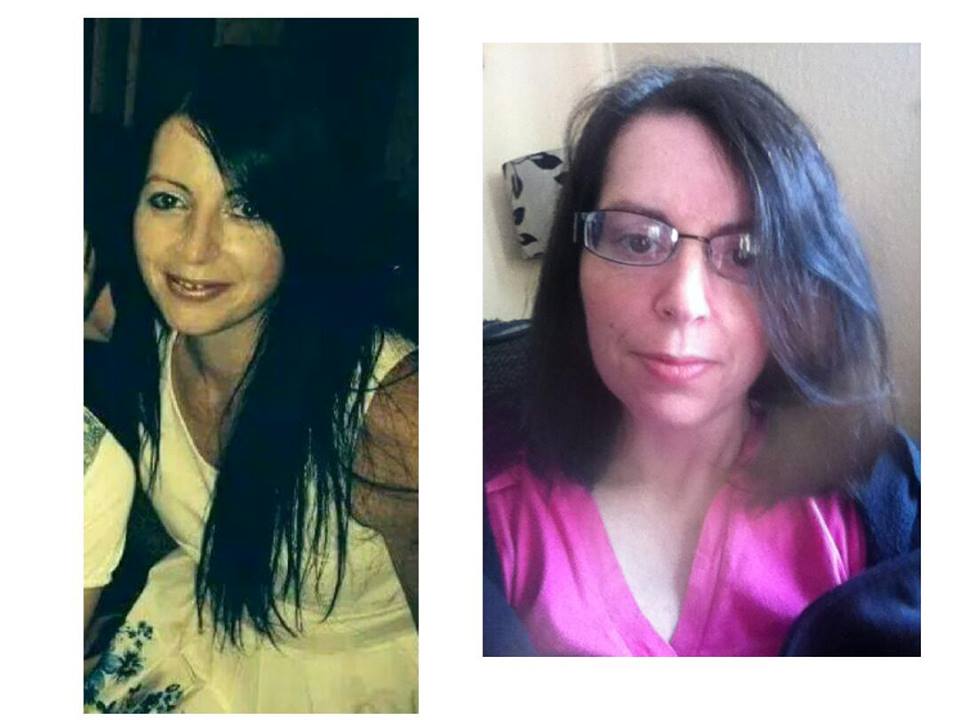
Before surgery, Lindsay had recommended I cut my hair, but since I learnt they would only need to shave a small area and that it would be hidden underneath then I was adamant I wasn’t cutting it! Fast forward to after surgery and the length was an issue, it was difficult to keep as I had restricted upper body movement, also the weight of it hurt my head and pulled at the scarred area. Lindsay took great pride in saying ‘I told you so’…several times! I had originally asked a friend (who is a trained hairdresser) to cut it, but I wasn’t up to sitting in the hairdressers so Lindsay offered to cut it! Call me mad/stupid but I was that desperate to have it cut I agreed! She spent two minutes on google before chopping it into a bob with a pair of kitchen scissors! Reluctantly I had to admit she did a good job! Here’s a photo of my hair before surgery and after Lindsay’s handy work!
After arriving home, I received an array of beautiful get well gifts from my colleagues! I was overwhelmed and moved to tears by their kindness. Here’s a wee picture of those gifts which were a beautiful bouquet of flowers, two hanging baskets and the brackets to hang them on, a voucher for afternoon tea for two and a Debenhams gift voucher and another bunch of flowers from the home…you can understand why I was so overwhelmed!

My colleague Dot had her long service award ceremony at work on the Thursday after I got home, she had been such a huge support to Lindsay and myself I was determined I would attend. It felt amazing to see all my colleagues and residents that day and I couldn’t wait for the day I would get back to work. At the ceremony there was a barbeque and it smelt wonderful but unfortunately barbeque food doesn’t really lend itself to a soft diet! So I drank my slightly thickened orange juice instead…mmm!
I found a recording of my voice from September 2014 on my phone and I couldn’t believe how slurred my speech was, in parts of that recording I couldn’t even understand myself. My slurred speech was one of the first things my doctor picked up on, even though it wasn’t one of the symptoms I had gone to him with – as I had always assumed, as did others, that I had a speech impediment – but he said that it could be connected with my other symptoms which made him believe it was a neurological problem.
I had been home from hospital ten days when the physiotherapist paid me a home visit to assess me with regards attending the rehabilitation unit. She was surprised at the level of my mobility and determination to get around the house! She explained to me that by attending the rehab unit I would receive several different therapies all under the one roof. I was looking forward to getting started on the road to recovery.
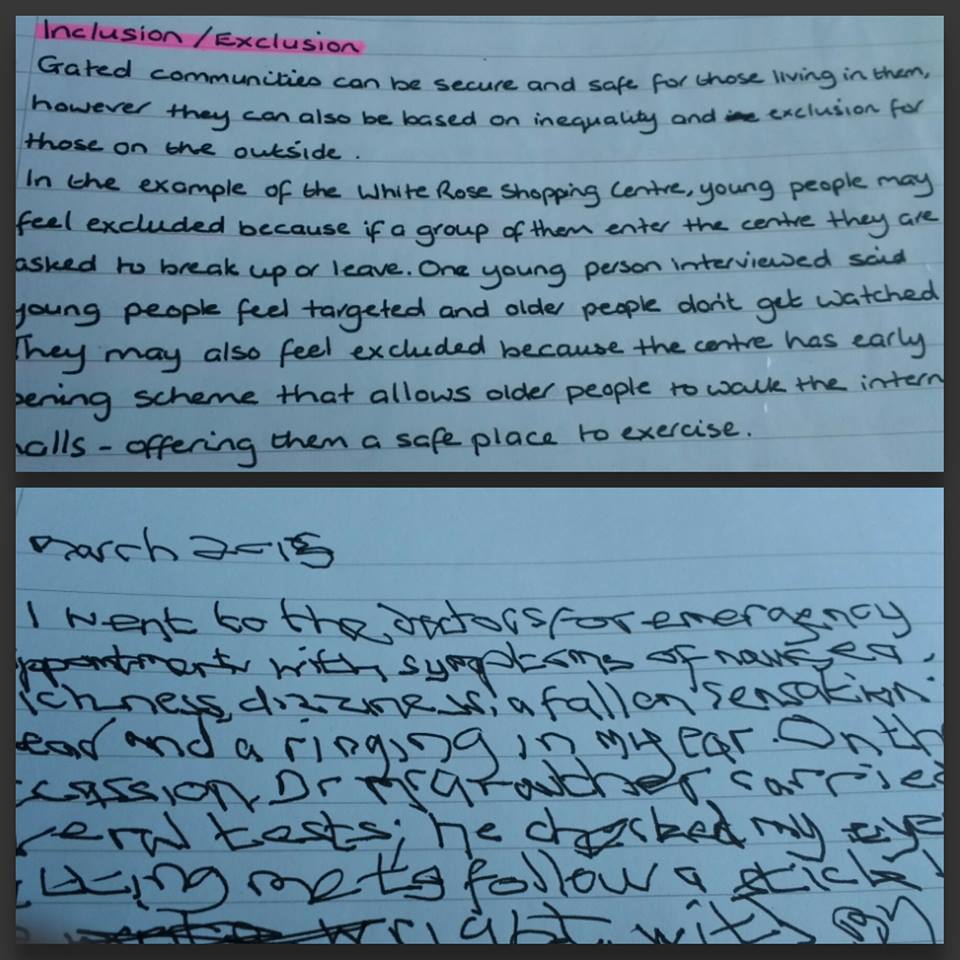
At the rehab unit I tried to do a ‘heal to toe’ walk for the first time since surgery (I was asked to do it several times before surgery as a neurological test, and each time I stumbled off balance). I was very unsteady and my leg became very shaky/jerky, ataxic. I started to panic as I’d not experienced that level of uncontrolled movement since before surgery, and a little part of me worried the cyst had regrown. But the physiotherapist had me repeat it several times, and the shaking reduced. She explained to me that my brain was processing something new – as it had been the first time the brain had been asked to do this movement since surgery – and that’s why it was such an uncontrollable shake, but once I had repeated it, although signs of ataxia were still there, my movements were a little bit more controlled. My brain was having to be taught how to coordinate my movements from scratch. This proved to be the case with writing as well. When I first went to write something after surgery I was shocked at how hard it was to write and how messy it was! Here’s a picture to illustrate the difference between my normal writing before surgery and my first attempt at writing after surgery!
Nine weeks after surgery Lindsay drove me back up the Western General Hospital in Edinburgh to see an ophthalmologist with regards my double vision, although the prism glasses were working I was still hoping my sight would improve. Six weeks previously my prism had been fourteen, now it was only nine which showed my sight WAS slowly improving! The consultant told me that had there been no signs of improvement then he doubted there ever would have been, but now he thinks there could be more!
After we had returned from Edinburgh I couldn’t understand why I was so tired. Lindsay had obviously done the driving and the examination hadn’t been too extensive or taxing. I happened to mention it to my physiotherapist and she explained that the brain has the capacity to filter out so much of what we see and hear (a bit like the junk folder in email!). However, my brain can no longer filter sights and sounds, and so for the whole journey my brain was trying to process everything it saw and heard, essentially overloading itself causing me to feel so exhausted. I was slowly beginning to realise there was more to my brain injury and post-surgery recovery than I had originally comprehended.
Miss Independent, Kidnapped and Homeward Bound (part 8 of I’m a 40-year-old blogger virgin!)
As we were leaving Edinburgh the ambulance had to pull over to let me lie down on the stretcher, I’d insisted that I wanted to sit on a chair for the journey – against the advice of the staff – but after only a few miles I had to admit defeat as I was getting sore and tiring trying to remain seated! Then for the rest of the journey I slept! I woke up as we were entering Dumfries and the familiar sights around me were overwhelming, I wanted to cry in relief at being closer to home. As I was wheeled through the front doors of Dumfries & Galloway Royal Infirmary (DGRI) the first person I saw was Emma, a good friend of mine, and the tears came!
My bed wasn’t ready when I got on the ward so I waited in the relative’s room and a colleague surprised me by rushing up to visit me as soon as she heard I was back on home soil! It was great to hear all the news of work, I’d thought of work often and missed it.
I was finally given a bed in a single room with en suite facilities! When I was in Edinburgh I was only allowed to mobilise with the assistance of a nurse or carer and with the help of Mavis (my walking aid – she was introduced in part 7!) but when I got to DGRI I told them I would be okay going to the bathroom on my own as, unlike Edinburgh, it was in the same room, so I blagged my way to become Little Miss Independent!
I had thought my days of loss of dignity had passed, but sadly not! Because I had been transferred from another hospital they had to take a swab to check for MRSA. That doesn’t sound too bad – until I learned the swab would be from my bottom and would be done by a young student nurse, time to cringe and die inside again!
Later that day a support worker gave me a menu for dinner and I noticed it had more appetizing meals on it than Edinburgh, in Edinburgh my menu differed from my roommates and I only ever saw soft options, so I was getting excited about having ‘proper’ food – until this woman breezed in to my room, took the menu out of my hand and highlighted the limited food I was allowed to choose from, and it didn’t include any of the appetizing food that had originally caught my eye! ‘This woman’ turned out to be the speech therapist, and although I had talked my way in to being able to mobilise on my own I wasn’t going to argue with her when it came to my swallowing, the fear of choking again was still a huge concern of mine.
17 days after surgery I discovered something strange…I couldn’t blow my nose! I’m not too sure why, but it was quite bizarre! Each time I tried the only thing that happened was air would escape from my mouth. When Lindsay came to visit me that evening I told her about it and I proceeded to demonstrate how I couldn’t blow my nose and how, instead, the air just blew out of my mouth…only on this occasion the air escaped from my bottom instead! Lindsay was highly amused and still laughs about it today, thankfully nobody else witnessed it!
The ward I was on was a mixed ward, one side was acute rehabilitation and the other side was care of the elderly. On my first night I felt like I’d been transported back to work (I work in a dementia unit), this wee old lady with dementia was running the nurses ragged, escaping out of the fire exit several times! She was sharp-tongued, slap happy and very wily! It made for an interesting night, I was use to the silence of the neurosurgical ward at Edinburgh! It made me want to put my work hat on and help!
On the second night I had quite a few visitors, it was a great pick me up to have the support and love of my friends. Also on the second night, the wee old lady got up to her antics again! And so the following day the nurses asked if I wouldn’t mind changing beds with the old lady as they felt they would be able to keep a better eye on her as the single room I was in was opposite the nurses station! So I found myself sharing a room with three ladies with dementia. This really put me in to work mode and I found myself pressing my buzzer a lot whenever I felt the ladies needed assistance but were unable to buzz themselves.
I was getting bored and restless so I tried to persuade Lindsay – for the second time – to bring my Open University study material! I had originally asked her to bring it to me when I was still in Edinburgh, what I thought I was going to do with it I don’t know…I could barely see faces never mind try to read! And I tired after a thirty minute visit so how I thought I would have the energy to concentrate and take any of it in! Sensibly, Lindsay put her foot down and refused to bring it to me!
On the Saturday – my 20th day in hospital – Lindsay kidnapped me! She’d brought along our dog Dexter, I was so excited to see him but sadly I couldn’t compete for his attention with the rabbits that were on the hospital grounds! We took a drive to the riverside (about two miles away from the hospital) and I toddled along a short path to the river and sat on a bench – in my pyjamas I should add! – and watched Lindsay throw sticks in the river for Dexter. I was overcome with emotion as I watched them, it seemed so long ago since we’d been together as a family. That night as I lay in bed reflecting on the day and on the journey I’d been on over the last couple of weeks I got tearful and I just wanted to return home now.
On the Sunday I told Lindsay to take a day off from visiting me and get herself to the pub! Except for three days in Edinburgh, she had visited me every day (one day she wasn’t well and the other two days I was waiting to be transferred, they fell through but it was too late for her to travel up), so she needed and deserved a day off to relax and recharge her batteries. I wasn’t alone though, Lesley and Dot came to visit me. Dot asked me if there was a chance I would be out for Thursday, as it was her award ceremony at work for her long service. I told her if I was still in I would get Lindsay to kidnap me again as I didn’t want to miss it!
As it turned out I didn’t need kidnapped because on the Monday – three weeks to the day since my operation – I finally received the news I’d been longing for, I was able to go home that afternoon! After Lindsay had settled me on the sofa at home she went to collect Dexter from her parents. I’ve two things to tell you about Dexter, firstly, it’s customary for Dexter to jump all over you and make a fuss if you’ve only been away from him for twenty minutes doing some shopping! And secondly, he never climbed up onto the sofa. However, as he came round the side of the sofa and saw me sat there, he very gently climbed up beside me on the sofa and gently lay his head against my chest. It’s as if he instinctively knew that mummy was poorly and he had to be gentle. It brought a tear to my eye as I sat at home with my family either side of me.
Small World, Big Milestones and Goodbye Edinburgh! (part 7 of I’m a 40-year-old blogger virgin…!)
As I was wheeled in to a ‘normal’ room from the high dependency unit I heard a familiar voice, one that I never imagined I would hear again, and if I’m honest, not one that I particularly wanted to hear again! My first reaction was I must be hallucinating again! But after the initial few minutes of hearing her voice turned into hours, I came to the conclusion that, I unfortunately wasn’t hallucinating it! I’m going to call this person ‘Ms S’, she was a former resident at my place of work, and at that time, she had a very challenging and demanding personality, and this continued to be the case here in Edinburgh! I couldn’t believe my misfortune at having her as a neighbour, all I wanted/needed was peace and quiet to recover, and all I got was a buzzer happy, chronic complainer in the bed next to me!
It turned out to be the ward of small worlds as the woman in the bed opposite me (who I’d never met before) knew my partner, my best friend and was a cousin of my ex mother-in-law!
On the Monday (one-week post-surgery) the physiotherapists who had visited me on Friday returned. At their last visit they had helped me to stand (not very successfully!), today they wanted me to try take a few steps. As they helped me to my feet I was unsteady, but I was determined to take a step. With the physiotherapists either side of me holding my arms, I managed to walk from my bed to the ward door (about fifteen feet) and back!
Also on Monday I was visited by my best friend Jill, we have been friends for 25 years, and despite all the pain and trauma of the last week, I turned into an immature giggling school kid – as is the usual when we are in one another’s company! I think the immaturity and giggles started the moment I told her that she had sat on my ‘pee bag’! It was great to see her and it really lifted my spirits.
Tuesday proved to be an eventful day! The speech therapist was pleased with the progress of my swallowing, she had been visiting every day trying me with different food and drink consistencies, and although I still had a feeding tube in, she decided I was ready to try puréed food. Now maybe most people would get excited at the thought of a meal after eight days of being fed through a feeding tube, but, some residents at my work are on puréed meals, and trust me when I tell you they are anything but appetizing! So although it was a milestone, my stomach wasn’t celebrating at the thought! Here’s a photo of that first meal. This picture was me finished with the dish, I couldn’t force feed myself anymore of it…and that wasn’t because I was having trouble with swallowing, I just couldn’t stomach it! Another lesson learned for when I return to work to those residents who have to eat this every day! And in case anyone was wondering what it was, it was corned beef hash!

Another milestone from that Tuesday was I had the catheter taken out! (Otherwise known to my friend Jill as a pee bag!) Once the catheter was out I had my first trip to the bathroom where I got to look at myself in the mirror for the first time. But I couldn’t see myself, my vision was too blurred all I could see was the outline of my face but not any detail, it was a bit unnerving and made me worry that I might be left like that. I raised my concern with staff and an appointment was made for me at the eye clinic.
And the final milestone for that day was I had my stitches taken out! If you’re squeamish you might want to quickly scroll past the next picture! But for those who aren’t faint-hearted, I decided to include a photo of my wound just after the stitches had been taken out!
![photo 1 [2736]](https://myarachnoidcystjourneydotcom.files.wordpress.com/2016/07/photo-1-2736.jpg)
When the consultant and his team did their rounds on the Wednesday they were really pleased with my progress and were talking about the possibility of me going home. I was so excited at the thought of being back home with my partner Lindsay and our dog Dexter! I told the speech therapist and physiotherapist the good news. Unfortunately, they didn’t share my enthusiasm, the speech therapist was concerned that I still had the feeding tube in and she had arranged for me to have a videofluoroscopy swallow assessment (a video x-ray of my swallow). The physiotherapists were also concerned as I was still unable to walk without their assistance and they felt there was still much more to be done before going home could be considered. They said that they wanted to give me the best start at the beginning of my recovery so that I can become the best I can in my long-term recovery. They went to talk it over with the consultant and, as a result, going home was put on hold. At the time, I felt absolutely deflated and if I’m honest I was angry at them for over-ruling the consultants decision. When I look back on it, knowing what I know now about the early days of recovery being crucial, I am grateful for their care and concern and completely respect what they did.
Thursday proved to be a busy day! Firstly, I was taken to the physio gym for the first time! Only to be told all I would be doing would be standing in front of the plinth and stacking plastic cups on top of each other at different distances on the plinth. I was hoping to go on a treadmill or something to improve my walking! (Again, with hindsight, I now realise the ridiculousness of my expectations!). So with a slightly petted lip I set about building a plastic cup tower, only to discover that if I bent too far to try to reach the plastic cups (which had been moved out of easy reach) I toppled over. And that was the point of the exercise, it wasn’t a simple case of practice walking and I’d be okay, my entire ability to balance was off. Another point to the exercise was to test my coordination, and as I reached for the cups I would miss picking them up, my arm would either over/under-shoot the cup or go to the left or right of it, it took a lot of concentration to coordinate my movements. At the time I had no understanding of why this would be affecting my walking. If it was explained to me then I don’t remember, or maybe I didn’t comprehend what I was being told. I now have a better understanding of how, in order to be able to walk, your body continually needs to balance itself and coordinate limb movements.
After physio I had the appointment at the eye clinic. The appointment was in the out-patient clinic on the ground floor, I was taken down in a chair and left, I felt very self-conscious sitting in front of the general public in my pyjamas and fetching white support socks! The ophthalmologist told me the nerves had been damaged as a result of the pressure of my lying face down for so long during surgery. The damage was quite severe and I was told it was an unknown whether it would improve, or if it did improve, by how much. It was a wait and see situation. In the mean time I was given a black eye patch so as the double vision wouldn’t affect my efforts to walk.
In the afternoon I had an appointment at the speech and language department for the video x-ray assessment of my swallow. Just before I went to it, I had been trying to adjust my feeding tube myself as it had been knocked during the eye tests. I somehow managed to nearly pull it out! The nurse had to take it out and I begged him to leave it out! He said he would leave it out until I returned from my appointment, but because I wasn’t managing to eat the puréed food he would need to insert it again. I explained to the speech therapist what had happened and she said that I was able to leave it out on the condition that I ate and drank enough and she would monitor my food chart.
During the assessment I was asked to drink barium liquid, I’m a fussy eater so it takes me some time to pick up the courage to taste anything new, so I asked if I could dip my finger in it first, as I couldn’t just take a sip without knowing what it tasted like! To my relief it tasted nice! I know I would still have had to drink it even if it tasted awful but it was the unknown of what it was going to taste like that I hated! As I drank it, x-rays were taken of my swallow to get a better understanding of my swallow process.
The following day the speech therapist had a surprise for me! Instead of having to eat custard she wanted me to try something new…a custard cream biscuit! Proper food! At first I coughed on the crumbs so spat it out but I tried again with more success! I wasn’t quite ready to eat a packet of biscuits but it gave an indication of where I was at with regards consistency. She decided I was able to try a diet of soft foods instead of puréed food! She also had the results of my video x-ray. The results showed that I had weakness in my mouth and throat and a delay in my swallow (the weakness in my mouth made it hard to hold on to food and drink in my mouth and made it harder to chew food). But the encouraging news was that over the last ten days I had already made huge progress with my swallow. Hours after waking from surgery I was unable to hold a mouthful of water in my mouth and I choked as it went down the back of my throat as I had no swallow, so to come from that to being able to eat soft food and slightly thickened fluids in ten days was huge progress.
Later that morning I was taken to the physio gym. I was trying to walk a figure of eight around cones, if the physiotherapists hadn’t been standing next to me I would have fallen. It brought it home to me why I wasn’t ready to be sent home. I had made progress in walking – as long as it was in straight lines! We practiced walking and turning with crutches but I couldn’t coordinate taking steps and moving my arms with the crutches, so I was given a different walking aid. Ladies and gentlemen let me introduce you to Mavis (so named by my work colleague Sharon!)
![photo 2 [2738]](https://myarachnoidcystjourneydotcom.files.wordpress.com/2016/07/photo-2-2738.jpg)
Mavis turned out to be an absolute blessing, we became inseparable! She brought me a bit of independence, with the help of Mavis I was able to get up and sit in the chair next to my bed, I could walk to the bathroom instead of being taking in a wheelchair (although I still needed to buzz for assistance as I wasn’t allowed to go on my own). On the Saturday Lindsay and her mum, Lesley, took me a wee walk around the hospital with the help of Mavis! I was exhausted when I got back to the ward but happy with my little jaunt!
For the last two weeks I had needed assistance of some form to wash myself, it was a bed bath the first few days and then full assistance in the bath and shower. But on the Sunday the carer asked me if I wanted to try to shower myself and she would stand by in case I needed help, what an amazing feeling it was! But even though I was sat down in the shower I began to tire so she needed to step in to help rinse me, but I was grateful that she let me try even though she would have known it would be more time-consuming, I felt she was helping to promote my independence.
On the Monday (two weeks after surgery) the consultant again spoke of returning to Dumfries, but this time they didn’t talk about going home they suggested a transfer to my local hospital. I wasn’t too disappointed at not getting sent straight home, after I nearly fell in the gym and after a choking episode a few days ago, I decided I would rather wait a bit longer before going home because I didn’t want to put any worry or onus on Lindsay with regards falls or choking. Instead I set my sights on a transfer and was happy that I would be a step closer to home and it would mean Lindsay didn’t have the daily five-hour round drive to visit me, instead it would be a ten-minute drive across town!
On the Tuesday and Wednesday my transfer fell through, I admit to shedding a little tear on the Wednesday but then I made myself look at the bigger picture, I had been there seventeen days a few more wouldn’t hurt! By the end of the day I was told that the transfer was back on for Thursday, I was so excited I couldn’t sleep and I got myself up at six to pack my bags! At 8.30am my transport arrived and I was saying my goodbyes I got tearful, the staff had been outstanding. At my most vulnerable they had cared for me with respect, dignity and genuine care and I was so grateful for it all.
As I was ready to be wheeled out of the room the transport support worker asked me if the rollator (Mavis!) was coming with me and I said no it belonged to the hospital. At that point the ward sister stepped in and told me to take it and she wouldn’t tell if I didn’t! I was so grateful as I had been worrying there wouldn’t be one available in Dumfries. When we got to the lift at the end of the ward, the nurse who had taken care of me in the high dependency unit came running down the corridor shouting “wait”! She gave me the biggest hug and told the transport staff to take care of me as I had been her star patient! Needless to say I started crying again! And so it was with a thankful and somewhat heavy heart I said goodbye to ward 33, but I was looking forward to the next chapter in my recovery.
Hoists, Hallucinations and Goodbye High Dependency Unit! (part 6 of I’m a 40-year-old blogger virgin…!)
On the third day after surgery (Thursday) I was told I would have a bath, up until then I had only received bed baths which were painful as I was rolled from side to side and sat forward slightly, but I was also worried about the pain of being moved with a hoist to the bath. It was an unpleasant experience in the hoist and, as I suspected, painful too. I didn’t feel safe even though the sling that was used was a full-bodied one which is like a cocoon, I felt vulnerable; I think it comes down to feeling a loss of control over all your movements and needs. For the first time since surgery my hair was washed, it was a strange sensation as the nurse touched my head, it felt numb and yet painful at the same time, and even down to this day it still has a degree of numbness when it’s touched, but thankfully less painful. After the bath, the only way to dry me was on my bed and so I still needed to be rolled to be dried and to change the bed sheet, I was exhausted after it all.
On a side note, I’m a carer in a nursing home and as I reflect back on my experience of being hoisted and receiving full assistance with my mobility and personal care it gives me incredible insight in to what some of my resident’s experience on a daily experience.
During the first day’s post-op I would often hallucinate! When Lindsay came to visit me on the Thursday I told her she had just missed Alan, Ian and Kelly (good friends from Hull, England). I was convinced they had been to visit me that morning, however, when Lindsay asked for a bit more detail and I said they had arrived with her dad…she knew I was talking gibberish! Other examples of my hallucinations were I kept seeing the ward equipment – like monitors and over bed lamps – as dark, menacing monsters or spies! Also, there was a doctor who had shoulder length hair, and I was convinced that every time he entered the HDU he would introduce himself by saying: “Hi, my name is David, but I use to be known as Sarah”, bizarre and untrue (I asked a nurse a week later if I had imagined it or if was true!). My hallucinations also manifested themselves as auditory hallucinations. I often heard music being played through the walls, one night I couldn’t sleep for the ‘music’ and I asked the nurse if it could be turned down…only to be told there was no music playing!
It had been arranged that on Thursday afternoon Lesley and Allan (Lindsays’ parents) would travel up on the bus to visit me and then they would return home with Lindsay as it was her final day staying in Edinburgh. I felt sad that she wouldn’t be close by, but I was over the worst and our dog – Dexter – would be missing his mummy! And she continued to drive up to visit me on a daily basis for the next two weeks!
On the Friday I had a surprise visitor – this one was not a figment of my imagination! – my colleague and good friend Dot travelled up with Lindsay, it was a lovely surprise! Dot has since told me that when she saw me she got such a shock at how ill I looked and how wee and helpless I appeared. She also said she witnessed something beautiful, she told me that Lindsay was staring intently and smiled adoringly at me when she told me I was looking so much brighter. And Dot said I was looking at Lindsay and it looked to her as though I was searching Lindsays’ face and hanging on to her every word as if wanting to believe her loving reassurances. Dot said it almost brought her to tears but she didn’t want me to see her cry. Her support to Lindsay that day was worth more than anything money can buy and very much appreciated. Oh and apparently they went sightseeing too (in other words they got lost!!).
Later on that day I was visited by two physiotherapists who were there to help me to stand up. Up until that point I hadn’t given standing or walking much thought, I assumed I was being hoisted because I was too weak/tired and groggy to walk, it never occurred to me that there would be a problem. However, as I went to stand up my legs buckled, it was only because the physios were holding me on either side that I remained standing. I got a fright and I couldn’t understand why my legs wouldn’t support me. The physiotherapist told me not to worry, they would let me rest over the weekend and they would return Monday to try again.
On the Saturday the nurse had suggested she hoist me on to a chair so that I could surprise Lindsay! I was shocked at how such a simple task made me feel exhausted and even though I tried so hard to stay in that chair until Lindsay got there, I eventually had to admit defeat and asked to go back to bed before she arrived. But I managed it the following day and Lindsay and her mum were so pleased to see me sat in the chair as it represented progress on my part!
There were several times in my first week I would be told off by the nurse as I would try to tolerate the pain, one, because I’m stubborn and, two, because I didn’t want to bother her (because I had a feeding tube it wasn’t a simple ‘here’s a pill to swallow’ it was a bit more intricate at getting the medication through the tube, that’s why I thought I was being a bother!) but that would result in me leaving it too late and, just like on my first night, the pain seemed to go from being bearable to excruciating and would have me in tears. Believe it or not, it took me over a week to finally give up my stubbornness and my concern at bothering the nurses and ask for pain relief. Even now I still get it wrong and think I can manage the pain without taking medication!
I was asked by the consultant neurosurgeon if I felt up to being asked questions about my symptoms by two medical students, he said that although some of my symptoms were common to other illnesses my diagnosis was rare. I was more than happy to as it may help future doctors be able to identify a rare and life threatening case. During the rest of my stay I was asked several more times to be a ‘guinea pig’ for the students, it was fascinating listening to them fit the different symptoms together to try arrive at a diagnosis. Although no one arrived at the correct diagnosis of an arachnoid cyst on the brainstem, they were able to rule out what it couldn’t be, and one girl was able to say my brainstem had been compromised but she didn’t know what the cause was. It showed me how complex the brain is and what a vast amount of knowledge is needed by the medical students.
By the Sunday it was decided by the consultant neurosurgeon that I was now able to be transferred to a ‘normal’ room on the ward and out of HDU! I was happy because again it showed progress, but I was also a bit sad as I had grown close to the nurse in HDU and felt safe under her care.
The Darkest Day Of My Journey (part 5 of I’m a 40-year-old blogger virgin…!)
On the first night after surgery I was woken up regularly by the nurse for neurological checks, she became increasingly concerned with my breathing as it had become laboured and shallow. The nurse called the doctor, who, after observing me from the foot of my bed, told her just to continue monitoring me overnight. She gave me an oxygen mask which I kept lifting off and resting on the bridge of my nose much to her annoyance! As the night went on my breathing deteriorated a little more and I began panicking because I couldn’t breathe but that was only making the situation worse, so the nurse sat by my bed and kept offering reassurances and calmed me down, I drifted in and out of sleep until morning.
In my previous blog I mentioned I felt remarkably well after I came round from surgery, well that initial feeling was rapidly disappearing, I felt awful, I was struggling to breathe, I was throwing up and the pain in my head was sheer agony.
On the morning after surgery I started choking on my own saliva, I couldn’t cough to clear my throat as I had no coughing reflex and I couldn’t swallow as the nerves that controlled these actions were in ‘trauma’ from the surgery*, and I remember feeling an overwhelming sense of panic and dread as I couldn’t see the nurses and I wasn’t able to shout out for help. There was a young guy in the bed diagonally across from me, who thankfully saw my distress and struggle and called out for a nurse, the nurse called my name asking if I was okay, that is when I realised the nurse was only a few feet away from me attending to the patient in the bed next to me with the curtains shut, but I still couldn’t talk as I struggled to clear my throat and breathe. She came out to check on me and ran to my side, I can’t remember what advice she gave or if she intervened with some action but I was sick which helped clear my airways. It may sound melodramatic now as I type this, but it was a frightening experience and one I will never forget and still fear today, I had the horrific thought I was going to choke to death. Sadly, it wasn’t a one-off incident, this continued to occur over the next couple of days and was often resolved by my being sick.
* the area of the brain that is responsible for initiating reflexes for swallowing and coughing and is also responsible for regulating breathing is the medulla oblongata, the lower part of the brainstem, which is where my cyst had been, which explains the ‘trauma’ to the nerves housed in that area and also why I was having difficulty with my swallowing and breathing.
Later on that morning the nurses gave me a bed bath, I felt an overwhelming sense of helplessness, vulnerability and embarrassment (in my previous blog I had hinted at what could be more embarrassing than going to hospital with hairy legs…well this was just one of many of those things). However, the nurses’ sensitivity and attentiveness helped to relieve some of my feelings.
During the day I was visited by a speech and language therapist to assess my swallowing. She gave me some water to drink, but I couldn’t take a sip of water without choking, it’s hard to describe not being able to swallow when it’s something we do hundreds of times through the day without really thinking about it. But as I took that sip of water I couldn’t activate the swallowing mechanism, neither could I hold on to the water in my mouth, which resulted in the water trickling down my throat, but without the swallow reflex it caused me to choke (similar to when your food or drink goes down the wrong way).
The speech therapist decided I would need to have a feeding tube for the foreseeable future, I asked what a feeding tube involved and I didn’t like the answer very much, a tube would be fed through my nose in to my stomach! It turns out the procedure wasn’t so bad!
In the afternoon I was moved to another High Dependency Unit (HDU) on the ward, this one only required one nurse to stay in it at all times and had three beds.
When Lindsay came to visit me I was still upset by my breathing and choking incidents, and unbeknown to me at that time, Lindsay has since told me that when I was relaying the incident to her I had said to her I wish I had died. I have no recollection of saying that to her and I can’t remember feeling like that, but it saddens me to think she was staying over in Edinburgh on her own and had the burden of hearing those words.
I asked Lindsay to ask the nurse for a buzzer/call button as I had a fear of choking again, the nurse tried to explain that she would always be there as the HDU could never be left unattended, but nothing would relieve my fears because the nurse had only been a few feet away on the previous occasion but I had been unable to get her attention, and so Lindsay convinced them to let me have a buzzer. When she rang the HDU that night at about ten (she did every night) to see if I was settled she checked to make sure I had my buzzer! I slept with the buzzer in my hand all night!
During the night I began choking again and the nurse gave me suction to clear my throat, by the following night I was able to use the suction tube myself which gave me a wee sense of control over the choking fear. Over the next few days I was choking less but the fear of choking to death remained, and still does to this day.
The speech therapist continued to visit, but as I was still unable to swallow sips of water she tried a thicker consistency…cold custard! I detest custard, and cold custard is just the produce of the devil! It amused Lindsay no end that I was being spoon-fed cold custard! But despite the thicker consistency I was still unable to swallow (although I’m not sure if that was down to an impaired swallow reflex or I hated the cold custard!) so I had to continue with the feeding tube for my medication, fluids and food.
Happy Brain Surgery Anniversary – 1 Year Today! (part 4 of I’m a 40-year-old blogger virgin…!)
Wow I can’t believe it’s been a whole year since my surgery, it still feels surreal one year down the line! It seems rather fitting then that this blog writes about my surgery day on my first anniversary!
With only 72 hours until I went to Edinburgh for brain surgery I suddenly had the most horrendous thought…my legs needed shaved! What could possibly be more embarrassing than being seen with hairy legs? (it turned out quite a few things were more embarrassing but I’ll explain that at a later date!). By this point though I couldn’t control my arms and legs very well, they would often twitch/jerk at random moments and my movements were stilted and clumsy, so holding a sharp instrument against myself was not a good idea! That’s where my loving, patient partner came to my rescue!
I’ve a funny story to tell about my partner Lindsay, she wanted to stay in Edinburgh for a few days after my operation so she could be closer to hand for those first few days of recovery (we lived a four-hour round trip from the hospital). As her mum and I were browsing online for a B&B/hotel for her, she casually tells us not to bother booking anywhere as she would sleep in the back of the car with our dog – Dexter the black Labrador! I looked up thinking I would see a twinkle in her eye as she tried not to laugh at her own joke, but no, she was deadly serious! Needless to say it was a resounding no from her mum and I!
As operation day approached my only noticeable anxiety was finding it hard to sleep, but if you were to ask me at that time if I felt nervous about going for brain surgery I would have said no. To me it was just something that had to be done – no ifs, buts or maybes.
On Monday 20th April 2015 Lindsay and I set off to Edinburgh at the ungodly hour of 5am! As we approached Edinburgh I decided I would post a final message on Facebook, here is a copy of that post:

So even down to the final hours before surgery I refused to be sombre about the occasion! Everyone who knows me will tell you I am Christmas mad and so this post seemed very apt for me, my mentality was if these were to be my last words to my friends I wanted them to be fun and upbeat!
We were 15 minutes late for the ‘check in’ time we were given so I was met by a waiting neurosurgeon and taken into a cubicle for last-minute health checks by the nurse (blood pressure and temperature) and then given the all clear for surgery. I was wheeled down to theatre on a chair and as we approached the double doors to the main corridor leading to theatre that was where Lindsay and I had to say our goodbyes. As I turned to Lindsay to say goodbye I was overcome with emotion I couldn’t speak for the lump in my throat, for the last 4 weeks I had kept it together and had been big, brave and strong – for Lindsay as much as myself – but at that moment I admit to having a wee wobble – lousy timing emotions! I managed to squeak out “I love you” before I was wheeled away through the double doors and the tears began to fall. The porter put his hand on my shoulder and said that’s the part that gets everybody.
The next part is all a blur! I met with the anesthetist who I had met at my pre assessment, and she put a canular in, but what was said after that, I can’t remember! I thought I would remember counting backwards or something dramatic (I’m sure they do on t.v!) while the anaesthetic took effect but I don’t remember a thing! I had been told that after surgery I would be taken to an after surgery room to be brought round from the anaesthetic and several neurological tests would be done to make sure everything was as it should be, but I don’t remember that stage either. My first memory was of Lindsay looking down at me and I was in the high dependency unit (HDU), I remember thinking at that time “I feel remarkably well considering!”
The neurosurgeon came to visit me and told me there had been a complication during the procedure and as a result I had been in theatre for five hours instead of the expected three. Now that was of no consequence to me as I was out for the count for those five hours but my heart ached for Lindsay as I thought of the anxiety she would have felt waiting all that time for news, it must have been excruciating…as it turns out not so much because Lindsay had gone back to the car and fell asleep for most of it! (For those who don’t know Lindsay, napping is what she does best, especially under stress!).
The complication the neurosurgeon referred to was that the route they had originally taken to reach the cyst had not been successful, so they had to retreat and take a different route. They had to lift the cerebellum in order to see and reach the cyst and it had attached itself to some pretty important nerves (well it had had 39 years to make itself at home!) so it was never going to be possible for it to be removed completely, but they were pleased they had been able to remove as much as was safe to do so. And despite the original setback the surgeon had said that the operation had been a resounding success and no unnecessary damage had been knowlingly done to any surrounding nerves, tissue or muscles! After seeing first hand the position of the cyst she reiterated what she had said to me at our first meeting that she was surprised I could still walk, talk or swallow.
As I came round a bit more It dawned on me that I couldn’t see too well, my sight was blurred and I had triple vision, Lindsay told me later that when I looked at her my left eye was directed at her but my right eye was looking as far right as it could, she found it very disconcerting as she talked to me!
The neurosurgeon assured me that the damage hadn’t been caused by surgery itself in as much as no optical nerves were damaged during the procedure, rather the damage would have been caused by the pressure to my eyes as I lay face down for the five hours, and it would be an unknown as to whether it would improve and, if so, by how much (I’ve came to slowly understand and accept over the last year that a lot of the neurological deficits experienced after brain surgery are very much an unknown as to regards to whether they will improve and, if so, by how much).
After Lindsay left I settled down to sleep, I had an intravenous patient control pump (morphine) which allowed me to self-administer so that I could control the level of pain relief as and when I felt I needed it. I felt a niggle but didn’t bother pressing the button, the niggle grew to being a wee bit painful but again I refrained from pressing the button, I’d put up with a lot of pain before the surgery and so still didn’t think this warranted a dose of morphine. How wrong that proved to be, because from being a wee bit painful it seemed to jump all other rungs on the pain ladder and shot to the most excruciating and unbearable pain imaginable. After I pressed the button there was a period of time – called lockout time – in which I couldn’t press the button again, even if I did the pump wouldn’t dispense the medication. After what seemed like an eternity the pain started coming down to a tolerable level but I continued to monitor that button and as soon as the light came on (that meant it was ready to dispense again) I pressed it! There was no way I was going to try to be big and brave again after the pain I had just experienced!
I’m not sure how much time passed with me doing this but I must have fell asleep eventually!
*please feel free to visit my Facebook page:
https://www.facebook.com/myarachnoidcystjourney/


